Uveal melanoma is a cancer of the eye involving the iris, ciliary body, or choroid (collectively referred to as the uvea). It is known as melanoma (usually related to skin cancer) because it is still a cancer that arises from the melanocytes, the pigment cells that give color to the skin and the eye. Uveal cancer cells are known to carry a so called "class 2 signature" which ranks the metastatic cells as one of the more aggressive classes of invasive cells.
Recently, doctors at the Washington University School of Medicine in St. Louis conducted studies that show that drugs known as histone deacetylase (HDAC) inhibitors alter the conformation of the aggressive form of DNA in uveal melanoma, which changes the gene expression, which makes these invasive uveal cancer cells less aggressive. HDAC inhibitors have commonly been used to treat seizures.
One of the big problems with uveal melanoma is that once it has metastasized, it is basically a death sentence. The big difficulty that arises from these cells is that they are able to remain in a dormant state for months before becoming detectable, but at this point they have spread throughout the body. Even if the primary tumor is detected and removed, metastatic cells could have already spread and lay dormant. According to the article, Histone Deacetylase Inhibitors Induce Growth Arrest and Differentiation in Uveal Melanoma, "half of these [diagnosed] individuals will eventually succumb to metastasis, despite successful treatment of the primary tumor, indicating that they harbored subclinical micro-metastases at initial presentation." The purpose of the study was to find therapeutic agents that reverse the phenotypic effects of BAP1 loss in uveal melanoma.
Experimental Design
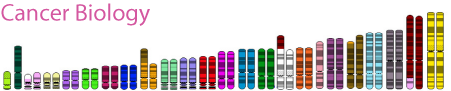
The experimental design was as follows. First off, in silico screens were done in order to identify a set of possible therapeutic compounds predicted to differentiate uveal melanoma cells. Gene Set Enrichment Analysis and Connectivity Map databases were used. Tumor samples were analyzed, and gene set enrichment analysis and connectivity mapping was done. Chemo-sensitivity assays were carried out along with mulitgene prognostic assays. qPCR was also done to determine mRNA levels. Finally, animal studies were also carried out by injecting mice with uveal melanoma cells re suspended in Cultrex. Among those therapeutic compounds evaluated were valproic acid (VPA) trichostatin A, LBH-589, and suberoylanilide. The big contenders however, were HDAC inhibitors. It was found that the HDAC inhibitors induced morphological differentiation, cell cycle exit, and a shift to a differentiated melanocyte gene expression in cultured uveal melanoma cells.
Conclusion
The BIG conclusion: HDAC inhibition blocks proliferation of uveal melanoma cells!
While some of the other tested compounds also inhibited proliferation of the uveal melanoma cells, they did not reduce the fraction of viable cells, or the clonogenicity of the uveal melanoma cells.
The figure above shows the effect of the HDAC inhibitors on uveal melanoma cell lines. The basic idea is that by adding the HDAC inhibitors, the number of cells per colony was reduced by a big percentage. It was found that the loss of the BAP1 protein sensitized the uveal melanoma cells to HDAC inhibitors allowing them to reduce the proliferation of the cells. the HDAC cells are then basically able to reprogram aggressive uveal melanoma cells to a low grade, differentiated state. It is mentioned that since there are already treatments involving HDAC for seizures, it should be easy to test it for cancer treatment as well as market it for cancer treatment.
Thoughts...
First off, I think that this is a good study in order to understand a bit more about how histone inhibitors work. I think it is a good starting point for using these inhibitors as possible cancer treatments. This also adds more insight about the possible inhibiting of cancer cells and the prevention of metastasis, which I think is the most important knowledge gained from this study. The knowledge that uveal cells can be reprogrammed to not proliferate and metastasize as an aggressive cell can provide, in my opinion, more insight into cancer cell metastasis.
In regards to actually marketing it and using it as an official cancer treatment, I think that a bit more research needs to be done. I tried looking for some other research that could support these finding and couldn't really find anything too conclusive. I really like the idea, but it seems a bit too good to be true. Then again that could just be my skeptical side.
I also would wonder about any side effects that could originate if administered as a cancer treatment. If it is already used as a seizure drug, could there be side effects in that cascade or system if implemented as a cancer treatment?
I think my overall conclusion is that it seems like the use of HDAC inhibitors has a lot of potential but it still needs to be double checked. I think that if it does turn out to be an effective way to treat uveal melanoma without any side effects based on its other treatments, then it would be a very efficient and easy drug to use and market because it is already approved and in the general public.
A little bonus...
I just thought that this picture was really cool and very clear.
References
http://www.sciencedaily.com/releases/2011/11/111128171222.htm
http://en.wikipedia.org/wiki/Uveal_melanoma
Washington University School of Medicine. "Drug may slow spread of deadly eye cancer." ScienceDaily, 28 Nov. 2011. Web. 14 May 2012.